Insurance Terms
What does that insurance term actually mean?
IN-NETWORK PROVIDER
Example:
Aria needs to see a specialist for an issue with her knee. If she visits a doctor who is in-network, the insurance company has negotiated lower rates for their services. As a result, Aria will pay a smaller copay or coinsurance for the visit. For example, the visit might cost her $30 instead of the full price of $100.
Definition
In-Network Provider: A therapist or clinic that has a contract with your insurance company, usually costing you less.
OUT-OF-NETWORK PROVIDER
Example:
Kendall sees a specialist for a consultation. Kendall's insurance has a network of providers but his doctor isn't one of them. Kendall's bill ends up being higher because his doctor was not one of the providers his insurance works with.
Definition
Out-of-Network Provider: A therapist or clinic that does not have a contract with your insurance, often costing you more.

PRE-AUTHORIZATION
Example:
Jamie is looking to see a specialist. However, before Jamie can be scheduled for an appointment by their doctor, their insurance first requires them to get pre-authorization.
Definition
Pre-Authorization: Approval from the insurance company that is required before starting certain therapies or procedures.

EVALUATION
Example:
Cyrus has been having difficulties in school, so Cyrus's parents take him in to see a therapist to get an evaluation done. The evaluation gives Cyrus and his parents a clearer understanding of any challenges and helps the therapist determine the best treatment plan.
Definition
Evaluation: A detailed assessment done by the therapist to determine your child's needs and set therapy goals.

PLAN OF CARE (TREATMENT PLAN)
Example:
Leah's been struggling with hand-eye coordination and grasping objects. In order to help Leah, Leah's therapist has created a treatment plan specific for her needs. The treatment plan targets goals and milestones for Leah in order to help improve her fine motor skills.
Definition
Plan of Care / Treatment Plan: A written plan created by the therapist outlining therapy goals and methods, often required by insurance.
CLAIM
Example:
Felicity visits her primary care doctor for a routine checkup. After the visit, her doctor's office submits a medical claim to her health insurance company for reimbursement. Felicity's health Insurance reviews the claim to determine how much they will cover, based on her policy. If the services are covered under her insurance plan, the insurance will apply the appropriate coverage for the costs.
Definition
Claim: A request sent to the insurance company to pay for therapy services.
SESSION LIMIT
Example:
Jane has a session limit for 30 visits a year. This means Jane's insurance will help cover up to 30 doctor or medical visits. After she uses the 30 appointments, the insurance will no longer be able to help cover the costs.
Definition
Session Limit: The maximum number of therapy sessions covered by your insurance each year.

DEDUCTIBLE
Example:
Logan has a deductible of $300, which means his insurance won't pay anything until he has paid $300. If Logan's treatment is $1000, Logan would pay $300 of it and his insurance would pay the rest, which would be $700.
Definition
Deductible: The amount of money you must pay for healthcare services before your insurance starts to pay.
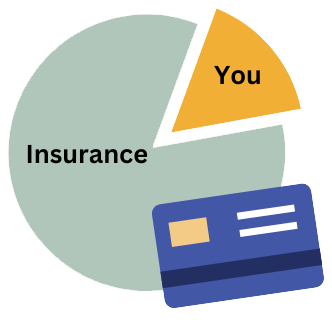
coinsurance
Example:
Caleb has a surgery that costs $5,000, and has already paid his deductible. Caleb will pay 20% of the bill, which is $1,000. Caleb's insurance will cover the remaining 80%, which is $4,000.
Definition
Coinsurance: The percentage of the therapy cost you have to pay after meeting your deductible, such as 20% of each session.
OUT-OF-POCKETMAXIMUM
Example:
Lily's OOP max is $4000, which she can pay off through copays, deductibles and coinsurances. Once Lily has paid off her total of $4000 her health insurance will begin to pay for 100% of her costs for covered care.
Definition
Out-of-pocket maximum (OOP Max): The most you'll have to pay for therapy and other healthcare in a year. After you reach this limit, insurance pays 100%.

denial
Example:
Lucas has a therapy appointment. After the appt, his therapist submits a notification (ie. claim) to Lucas's insurance that therapy occurred. In review of the plan Lucas has, his insurance company denies the claim because therapy services were not covered in his plan. They refuse to cover the cost of the therapy appt. Lucas must now either appeal the denied claim, or pay out-of-pocket to cover the costs.
Definition
Denial: When the insurance company refuses to pay for a therapy service.
apPeal
Example:
Daniel sent in a claim to his insurance to have his doctors bill paid for. However, his insurance company denies his claim, refusing to pay for his appointment. Daniel sends in an appeal by sending in more documents describing the procedures and medications he got. Daniel hopes his insurance company will reconsider after sending in the appeal.
Definition
Appeal: A process of asking the insurance company to review and change a denial decision.
REIMBURSEMENT
Example:
Melody goes to therapy for a month, with each session costing $120. Melody pays for 4 sessions, totaling $ 480. After the sessions, Melody contacts her insurance company to submit a claim in order to be reimbursed. Her insurance company reviews the claim and reimburses her for 80% of the total cost, which is $384.
Definition
Reimbursement: Money your insurance pays you back if you've already paid for therapy out-of-pocket.

